A recent study presented at Digestive Disease Week (DDW) 2025 reveals a concerning increase in anal cancer diagnoses, particularly among older white and Hispanic women. Anal cancer, though rare, is becoming more prevalent in demographics not traditionally considered high-risk.
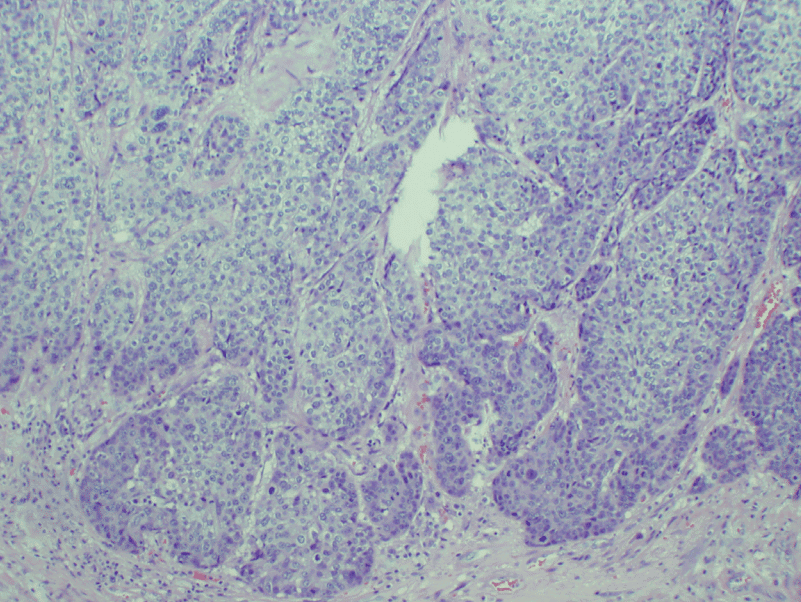
Anal cancer affects the anus, the opening at the end of the digestive tract. Common symptoms include bleeding, itching, pain around the anus, lumps, mucus discharge, and changes in bowel habits. These symptoms are often mistaken for less serious conditions like hemorrhoids or anal fissures, potentially delaying diagnosis.
The study analyzed data from 2017 to 2021 and found that anal cancer rates increased by 2.9% for women and 1.6% for men. The most significant rise was among white women over 65, with a 4.3% increase, and Hispanic women in the same age group, with a 1.7% increase. These groups are not typically considered high-risk, highlighting a shift in the disease’s demographic impact.
Human papillomavirus (HPV) is responsible for approximately 90% of anal cancer cases. The HPV vaccine, introduced in 2006, is effective in preventing infections that can lead to anal and other cancers. However, many older women were beyond the recommended vaccination age when the vaccine became widely available, leaving them more susceptible to HPV-related cancers.
Dr. Ashley Robinson, the study’s lead author, emphasizes the importance of promoting HPV vaccination and updating screening guidelines to include older women. Currently, anal cancer screening is recommended for high-risk groups, such as individuals with HIV or those who are immunocompromised. Expanding these guidelines could aid in early detection and treatment.